Convenience meets expertise. Here's why Medicspot is your perfect healthcare partner.
Abscess or boil symptoms include swelling, redness, pain, and the formation of a pus-filled lump. It feels tender, warm, and painful, with potential throbbing sensations, and may cause discomfort during movement or pressure.

An abscess, also known as a boil, is a common skin condition that results from an infection in a hair follicle or oil gland. It appears as a painful, swollen lump filled with pus, and it can occur anywhere on your body. While most abscesses are not serious, they can cause discomfort and pain.
Abscesses are usually caused by bacteria, most commonly Staphylococcus aureus, entering the skin through a cut, scrape, or hair follicle. Poor hygiene, friction, and compromised immune systems can increase the risk of developing abscesses.
Abscesses typically start as a tender, red bump that becomes more painful over time. The affected area often becomes swollen and warm to the touch. As the infection progresses, the center may fill with pus. In some cases, there may be a mild fever. Eventually, the abscess may open and drain, releasing the pus and providing relief.
Antibiotics may also be prescribed to help clear the infection. Over-the-counter pain relievers can help manage discomfort.
Acute bronchitis is inflammation of the bronchial tubes, causing cough, chest discomfort, and shortness of breath. Symptoms include cough with or without mucus, fatigue, and mild fever. It feels like a chest heaviness and persistent irritation.
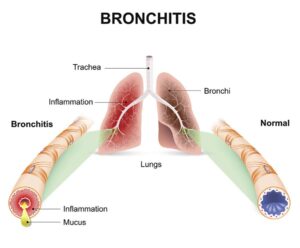
Bronchitis is an inflammation of the lungs, specifically of the bronchial tubes (which permit air to enter the lungs) in the lower respiratory tract. It occurs in two types:
• Acute bronchitis, which generally lasts for 1-3 weeks
• Chronic bronchitis, which is characterized by recurring symptoms over a period of months.
Acute bronchitis is a common condition caused by viral and bacterial infections. In most cases, symptoms are mild, but acute bronchitis may progress to viral pneumonia in some patients. We prescribe acute bronchitis antibiotics to help bacterial infections. In some patients, bronchitis medications cause side effects that can include upset stomach and vomiting. Be sure to inform a Call-On-Doc provider if you are experiencing side effects or allergic reactions in connection with your bronchitis treatment.
Persons suffering from acute bronchitis are usually advised to avoid tobacco smoke (including secondhand smoke) or exposing themselves to other airborne irritants. Some find it helpful to use an indoor humidifier to moisten indoor air. To recover faster, you should get plenty of rest and drink plenty of fluids.
Abscesses are usually caused by bacteria, most commonly Staphylococcus aureus, entering the skin through a cut, scrape, or hair follicle. Poor hygiene, friction, and compromised immune systems can increase the risk of developing abscesses.
. Frequent cough
. Sore throat
. Chills
. Headaches
. Fatigue
. Mild fever
. Chest congestion
. Persistent wheezing
. Yellow or green mucus
. Whistling sound while breathing
. Sore ribs from prolonged coughing
Antibiotics may also be prescribed to help clear the infection. Over-the-counter pain relievers can help manage discomfort.
responds to substances such as pollen, pet dander, or certain foods. Your antibodies identify these allergens as bad for you, even though they're not.
How common are they?
Nearly 18 million adults in the United States have hay fever, or allergic rhinitis. At least 1 in 3 American adults and 1 in 4 children have allergies.
Doctors don’t know exactly how many adults are diagnosed with allergies for the first time. But nasal allergies affect more Americans every year, according to the American College of Allergy, Asthma and Immunology.
Whatever the case, allergies are all over, and they’re big business. They’re the sixth-leading cause of chronic illness in the U.S., according to the CDC. And they cost Americans more than $18 billion a year.

Chronic allergies are a widespread condition that affects millions of people worldwide. An allergy occurs when the immune system overreacts to a foreign substance that is typically harmless to most people. Some of the most common chronic allergies include hay fever (allergic rhinitis), eczema, drug allergies, and food allergies.
Allergies are typically caused by your body's immune system response to external stimuli, with many being seasonal or temporary based on the surrounding environment. The most common of these stimuli include:
. Pollen
. Dust Mites
. Mold Spores
. Animal Dander
. Cockroach and Rat Droppings
. Insect Venom
. Airborne Irritants
The symptoms of chronic allergies are often persistent and can be difficult to manage. Some people may experience severe or mild allergy symptoms, including:
Sinus Congestion - Blockage or stuffiness of the nasal passages.
Coughing - Allergic coughing is a reaction to allergens such as pollen, dust mites, or pet dander.
Persistent Sneezing - A reflex action that occurs when the nasal passages are irritated by allergens.
Itching - A common symptom of allergies that can affect the skin, eyes, nose, and throat.
Facial Congestion - Feeling of pressure, fullness, or tightness in the face, usually around the sinuses or nasal passages.
Urticaria - Also known as hives, this is a skin condition characterized by the sudden appearance of itchy, red, or white welts or bumps on the skin.
Chronic allergies can also lead to life-threatening symptoms, such as asthma attacks and anaphylaxis.
The treatment for chronic allergies and allergy medications depends on the severity of symptoms and your medical history. Some commonly prescribed medications for chronic and seasonal allergies include:
It is important to consult with a healthcare provider to diagnose your allergies and determine the best way to treat your allergies, as some medications may have negative interactions with others or have potential side effects due to undetected drug allergies.

Some conditions Amoxicillin can treat include but are not limited to:
1. DO NOT use this medication if you are allergic to amoxicillin or to any other penicillin antibiotic, such as ampicillin, dicloxacillin, oxacillin, penicillin and others.
2. Before using amoxicillin, tell your doctor if you are allergic to cephalosporins such as Omnicef, Cefzil, Ceftin, Keflex, and others. Also tell your doctor if you have asthma, liver or kidney disease, a bleeding or blood clotting disorder, mononucleosis (also called "mono"), or any type of allergy.
3. Amoxicillin can make birth control pills less effective. Ask your doctor about using a non-hormone method of birth control (such as a condom, diaphragm, spermicide) to prevent pregnancy while taking this medicine.
4.Take this medication for the full prescribed length of time. Your symptoms may improve before the infection is completely cleared. Amoxicillin will not treat a viral infection such as the common cold or flu. Do not share this medication with another person, even if they have the same symptoms you have.
5. Antibiotic medicines can cause diarrhea.
You should not use amoxicillin if you are allergic to any penicillin antibiotic.
To make sure this medicine is safe for you, tell your doctor if you have:
Skip the missed dose and use your next dose at the regular time. Do not use two doses at one time.
Get emergency medical help if you have signs of an allergic reaction to amoxicillin including:
Call your doctor at once if you have:
Tell your doctor if you are taking any other antibiotic, Allopurinol, Probenecid, Warfarin or Coumadin.
Cough and congestion often result from respiratory infections or allergies. Symptoms include persistent cough, chest tightness, and nasal congestion. It feels like irritation and difficulty breathing.

Cough and congestion are common respiratory issues most often characterized by regular irritation in the throat, regular expelling of fluid from the nose or mouth, and obstruction of one or both nostrils. Often stemming from viral or bacterial infections, irritants such as smoke and allergens can also trigger these symptoms.
While viral infections tend to resolve on their own, bacterial infections may necessitate antibiotics. Over-the-counter cough syrups, decongestants, steam inhalation, and prescribed medications from CallonDoc can offer relief.
Various factors contribute to cough and congestion, including viral and bacterial infections, irritants, and environmental conditions. Alongside dry air and exposure to dust or chemicals, common causes include:
Acute Bronchitis: Causes congestion and coughing by inflaming the bronchial tubes, leading to excessive mucus production and irritation, which prompts the body to cough as a natural mechanism to clear the airways.
Influenza: Infection of the respiratory tract leading to cough and congestion.
Allergies: Immune response to airborne allergens causing respiratory symptoms.
Sinus Infections: Inflammation and congestion leading to postnasal drip and throat discomfort.
Covid-19: Causes congestion and coughing by infecting the respiratory system, particularly the airways and lungs, leading to inflammation, increased mucus production, and a cough response as the body attempts to expel the virus and restore normal breathing.
Smoking: Exposure to toxins causing inflammation and discomfort in the respiratory tract.
Environmental Irritants: Dust, pollution, or workplace chemicals triggering respiratory symptoms.
Upper Respiratory Infections: Cause congestion and coughing by triggering inflammation and irritation in the nasal passages, throat, and airways, leading to increased mucus production and a reflexive response to clear the air passages.
Given the multitude of causes, cough and congestion symptoms can manifest in isolation or indicate an underlying issue. Common signs accompanying these symptoms include:
Persistent Cough: A continuous cough is a prevalent symptom, often causing discomfort.
Nasal Congestion: Difficulty breathing through the nose due to blockage.
Throat Irritation: A scratchy or sore throat can accompany cough and congestion.
Difficulty Breathing: Labored breathing or shortness of breath.
Chest Discomfort: Sensation of pressure or pain in the chest.
Excessive Mucus Production: Thick mucus contributes to congestion.
Headache: Some individuals may experience headaches alongside cough and congestion.
Treatment for cough and congestion depends on the underlying cause. For viral infections, symptom relief is the primary focus, with over-the-counter medications and self-care measures. Antibiotics may be prescribed for bacterial infections. Adequate rest, hydration, and respiratory support, such as humidifiers, aid recovery.
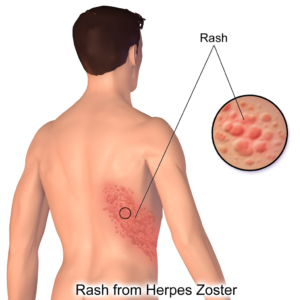
A cold sore is a group of tiny, painful blisters caused by the herpes simplex virus (HSV). They’re also called fever blisters or herpes simplex labialis.
Up to 90% of people around the world have at least one form of HSV.
The symptoms are usually the most serious the first you time you get cold sores. A first-time cold sore can make a child seriously ill.
After the first outbreak, your body should make antibodies, and you may never have another infection. But many people get cold sores that come back.

Cold sores, also known as fever blisters, are a common viral infection caused by the herpes simplex virus (HSV). These small, fluid-filled blisters typically appear on or around the lips, but they can also manifest on the nose, chin, or cheeks. Cold sores are highly contagious and can be transmitted through direct contact with the blister or through saliva.
The initial outbreak of cold sores is often preceded by a tingling or burning sensation, which is followed by the formation of small, red bumps. These bumps then evolve into painful blisters filled with fluid. After a few days, the blisters burst, leaving behind open sores that gradually crust over and heal within a week or two.
Although cold sore outbreaks are generally harmless, they can be uncomfortable and unsightly. The primary infection with HSV usually occurs during childhood or adolescence, and the virus remains dormant in the body. Factors such as stress, fatigue, hormonal changes, and a weakened immune system can trigger a cold sore outbreak.
You catch HSV when you come into contact with people or things that carry the virus. For instance, you can get it from kissing someone who has the virus or from sharing eating utensils, towels, or razors. Two types of the virus can cause cold sores: HSV-1 and HSV-2. Both types can also cause sores on your genitals and can be spread by oral sex.
Type 1 usually causes cold sores, and type 2 mostly causes genital herpes, but either can be found in both areas.
Certain things can trigger an outbreak, including:
. Some foods
. Stress
. Fever
. Colds
. Allergies
. Fatigue
. Sunburn or being in strong sunlight
. Dental work or cosmetic surgery
Cold sores are most likely to show up on the outside of your mouth and lips, but you can also get them on your nose and cheeks.
You may get cold sores as late as 20 days after you’re infected. The sore might appear near where the virus entered your body.
Cold sores happen in stages:
You have a tingling, burning, or itching feeling.
About 12-24 hours later, blisters form. The area becomes red, swollen, and painful.
The blisters break open and fluid comes out. This usually lasts 2 or 3 days.
A scab forms on the sore. It might crack or bleed.
The scab falls off.
In combination with antivirals like Acyclovir and Valacyclovir, cold sore treatment primarily focuses on managing and reducing the severity and frequency of outbreaks, as well as alleviating symptoms. While there is no herpes cure, the condition can be managed down to a dormant state per each flair-up through treatment and habits that involve lowering stress, reducing spread, keeping the flair-up site clean, etc.
COVID-19 is a disease caused by SARS-CoV-2 that can trigger what doctors call a respiratory tract infection. In early 2020, the World Health Organization identified SARS-CoV-2 as a new type of coronavirus. The outbreak quickly spread around the world. It can affect your upper respiratory tract (sinuses, nose, and throat) or lower respiratory tract (windpipe and lungs).
It spreads the same way other coronaviruses do, mainly through person-to-person contact. Infections range from mild to deadly.
SARS-CoV-2 is one of seven types of coronavirus, including the ones that cause severe diseases like Middle East respiratory syndrome (MERS) and sudden acute respiratory syndrome (SARS). The other coronaviruses cause most of the colds that affect us during the year but aren't a serious threat to otherwise healthy people.
COVID-19, short for "Coronavirus Disease 2019," is a highly contagious respiratory illness caused by a coronavirus known as SARS-CoV-2. Discovered in 2019 and responsible for the 2020 global pandemic, the virus is known for its aggressive spread and its symptoms that target the respiratory system, in addition to it targeting a person’s sense of smell and taste. Left untreated, severe cases can lead to pneumonia and acute respiratory distress syndrome (ARDS), posing a significant threat, especially to the elderly and those with underlying health conditions.
Covid-19 primarily spreads from person to person through respiratory droplets when an infected individual coughs, sneezes, talks, or breathes. It can also spread by touching surfaces contaminated with the virus and then touching the face, especially the eyes, nose, or mouth.
The main symptoms include:
. Fever
. Coughing
. Shortness of breath
. Trouble breathing
. Fatigue
. Chills, sometimes with shaking
. Body aches
. Headache
. Sore throat
. Congestion/runny nose
. Loss of smell or taste
. Nausea
. Diarrhea
The virus can lead to pneumonia, respiratory failure, heart problems, liver problems, septic shock, and death. Many COVID-19 complications may be caused by a condition known as cytokine release syndrome or a cytokine storm. This is when an infection triggers your immune system to flood your bloodstream with inflammatory proteins called cytokines. They can kill tissue and damage your organs. In some cases, lung transplants have been needed.
With most cases of Covid-19 resulting in mild symptoms, most examples of Covid-19 treatment will include plenty of rest, hydration, nutrition, and avoiding activities that might strain the patient. In addition to that, patients are still asked to isolate so as not to spread the virus to those who might be vulnerable to it. For those approved to get prescriptions for Covid-19, Call-On-Doc additionally offers Paxlovid.

Disclaimer: We are general practitioners (family medicine), and do not specialize in Dentistry or Orthodontistry. We do not treat patients experiencing severe pain, fever, copious pus, facial or jaw swelling.
A result of bacterial or viral invasion of the ear, causing pain, hearing loss, and potential drainage. Symptoms include earache, fever, and irritability, especially in children. Ear infections may feel like pressure or fullness in the ear.
Otitis Externa (Swimmer's Ear) often develops after repeated exposure to moisture from swimming, sweating, and humid environments It usually affects only one ear causing pain, redness and itching.
Otitis Media (Middle Ear Infection) occurs when a bacterial or viral infection affects the nasal passages, throat, and eustachian tubes.
The middle ear is a small space behind your eardrum. It contains tiny bones that vibrate and help you hear. This part of your ear is supposed to be vented by air that passes into your nose and throat and through a passage called the eustachian tube. If anything blocks air from getting through, the middle ear can become damp and warm – a perfect breeding ground for germs.
In babies and kids, the eustachian tube is often very soft and has a hard time staying open. Allergies, post-nasal drainage, sinus infections, common cold viruses, and problems with the tonsils can all prevent enough air from passing into the middle ear.
If a doctor looks at your child's eardrum and sees that it's red and bulging, they'll diagnose them with an ear infection.
Your child may have:
-Fever
-Pain in the ear (babies will rub or pull on their ears)
-Vomiting and diarrhea (in babies only)
-Trouble hearing
-Crying or pain when sucking
-Loss of sleep or appetite
The most common trigger of an ear infection in kids is an upper respiratory infection, like a cold or the flu. These viruses can swell the eustachian tube so that air can't flow into the middle ear. Allergies to pollen, dust, animal dander, or food can have the same effect. So can smoke, fumes, and other environmental toxins. Bacteria can cause an ear infection, but usually these germs come after a virus or an allergic reaction. Bacteria can infect an already inflamed ear and cause other symptoms, like a fever.
The treatment of an ear infection typically involves a combination of approaches to alleviate symptoms and eliminate the underlying infection. In many cases, bacterial ear infections are treated with antibiotics to completely remove the infection and prevent long-lasting damage. However, in the case of mild and viral ear infections, the condition will typically resolve itself on its own. In some cases, physical interventions are needed when there is a blockage or fluid that will not drain
Food poisoning feels sudden with nausea, vomiting, abdominal pain, and diarrhea. Symptoms may include fever and dehydration. Noticeable discomfort, weakness, and rapid onset distinguish it. Those with it will feel weak and noticeably uncomfortable.

Food poisoning, also known as food borne illness, is a potentially serious condition caused by consuming contaminated food or beverages. It occurs when harmful bacteria, viruses, parasites, or toxins are present in the consumed food, which can result in various symptoms and health complications. Food poisoning can affect anyone, and the severity of symptoms can vary widely depending on the specific contaminant and the individual’s health profile.
Food can become contaminated at various stages of its lifecycle, including production, processing, cooking, or storage. Common causes of contamination include improper handling of food that exposes it to pathogens or parasites, cooking or reheating at the wrong temperature, and cross-contamination between raw and cooked foods.
Food poisoning can be caused by various microorganisms, including:
Bacteria, such as Salmonella, Escherichia coli (E. coli), and Campylobacter
Viruses, such as rotavirus, norovirus, and hepatitis A
Parasites, such as Cyclospora, Cryptosporidium, and Giardia
Toxins produced by bacteria, such as Staphylococcus aureus and Clostridium botulinum
Each contaminant can lead to different symptoms and health effects. The duration of food poisoning also varies. In most cases, symptoms are mild and resolve within one or two days without the need for medical intervention. However, some cases are more serious and require medical attention. This is especially likely in vulnerable populations such as young children, the elderly, pregnant women, or those with weakened immune systems.
Symptoms of food poisoning range from very mild to severe, and can take many different forms, including:
Food poisoning treatment primarily focuses on relieving symptoms, staying hydrated, and allowing the body to recover from the effects of the contaminated food. In most cases, food poisoning symptoms resolve on their own within a few days. Common steps to treat food poisoning thereby include:
Avoiding spicy, fatty, and dairy-rich foods
Consuming bland food when possible
Replacing lost fluids
Flu feels abrupt with fever, chills, muscle pain, and fatigue. Symptoms include cough, sore throat, and headache. Noticeable weakness, body aches, and respiratory distress may accompany.
Influenza, commonly referred to as the flu, is a highly contagious respiratory illness caused by influenza A or B viruses. It strikes mainly during the winter season, causing a range of symptoms from mild to severe. Schoolchildren are particularly susceptible due to their close contact in crowded environments, such as classrooms.
To reduce the spread of influenza, annual flu vaccination campaigns are critical. Vaccination not only helps reduce the severity of symptoms during flu season but also lowers the risk of infection and subsequent transmission. Additionally, promoting good hygiene practices, such as frequent handwashing and covering coughs and sneezes, can aid flu prevention.
Most commonly, symptoms start to show about 1 to 3 days after being exposed to the influenza virus. Fortunately, medications like antiviral drugs can help treat flu symptoms and shorten the duration of illness if taken within the first 48 hours of symptom onset. These medications work by targeting the virus's replication, reducing its impact on the body.
The flu, or influenza, is caused by influenza viruses that infect the respiratory system. These viruses belong to different types and strains, with the most common ones being influenza A and B viruses. The flu is highly contagious and spreads through respiratory droplets when an infected person coughs, sneezes, or talks. Additionally, the virus can also be contracted by touching surfaces or objects contaminated with flu virus and then touching the mouth, nose, or eyes. Over time, any flu virus can mutate and change over time, leading to new strains that may cause reinfection and different symptoms.
Fever or feeling feverish (not everyone will experience this)
Cough
Runny or stuffy nose
Sore throat
Muscle pains or body aches
Headache
Fatigue and weakness
Chills
Sweating
Nausea or vomiting (more common in children)
Diarrhea (more common in children)
Doctors often treat the flu with a combination of supportive care and antiviral medications. Supportive care involves rest, staying hydrated, and managing symptoms with over-the-counter pain relievers. Antiviral medications like oseltamivir (Tamiflu) or zanamivir (Relenza) can be prescribed, especially for high-risk individuals or those with severe symptoms. These medications can shorten the duration of the illness and reduce the severity of symptoms by inhibiting the virus's ability to replicate. Treatment is most effective when started within the first 48 hours of symptom onset.
Heartburn is an irritation of your esophagus, the tube that connects your throat and stomach. This leads to a burning discomfort in your upper belly or chest.
It's caused by acid reflux, which is when your lower esophageal sphincter (LES) muscle doesn't close properly, letting stomach acids back up into your esophagus.
You've probably had heartburn, and it’s usually not serious.
If you have it often, you may have something else called gastroesophageal reflux disease, or GERD. If you don't get it treated, GERD can sometimes cause problems, like:
Inflammation and ulcers in the esophagus
Hoarseness
Some types of lung disease
Barrett's esophagus (when your esophagus is damaged by acid reflux)
Heartburn Symptoms
Heartburn feels like a burning sensation in the middle of your chest and throat. You may also have:
Burning pain in your chest after you eat or at night
Pain that worsens when you bend over or lie down
A hot, acidic, bitter, or salty taste in the back of your throat
A hard time swallowing
A feeling of food "stuck" in the middle of your chest or throat
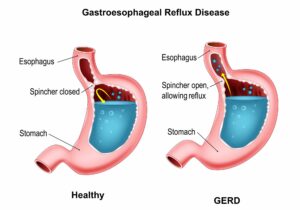
Heartburn symptoms can start when the lower esophageal sphincter (LES) valve at the bottom of your esophagus doesn't close correctly.
It should stay closed to keep food and stomach acids in your stomach. When you're eating, your LES opens so food can go into your stomach. Then it closes again. If it doesn't close, even just a little, or if it opens when it shouldn't, stomach acids can go back into your esophagus, causing heartburn pain.
We don't know what causes the LES valve to weaken, but it could be caused by eating big meals too often, if you're overweight, or you have a hiatal hernia (a hernia in your upper stomach that pushes through your diaphragm).
Heartburn risk factors
Certain foods can relax your LES or increase stomach acid, including:
. Tomatoes
. Citrus fruits
. Garlic and onions
. Chocolate
. Coffee or caffeinated products
. Alcohol
. Peppermint
. Foods high in fats and oils
Heartburn feels like a burning sensation in the middle of your chest and throat. You may also have:
Burning pain in your chest after you eat or at night
Pain that worsens when you bend over or lie down
A hot, acidic, bitter, or salty taste in the back of your throat
A hard time swallowing
A feeling of food "stuck" in the middle of your chest or throat
Intense, throbbing head pain with nausea and sensitivity to light and sound. Often accompanied by a growing difficulty in handling sound and light, the effects often involve incapacitating headaches, often requiring rest in a dark, quiet environment.

A migraine is an episodic neurological disease that causes severe headaches. Described by most people who experience migraines as having the worst headache of your life, it affects 17% of women and 6% of men.
Migraines are usually characterized by feeling throbbing or pulsating pain on one side of your head only, and experiencing a variety of other physical and neurological symptoms you wouldn’t expect from a regular headache.
A feeling of queasiness with nausea, dizziness, and possible vomiting during travel. Symptoms include sweating and pallor. Noticeable discomfort arises in moving vehicles or on rides, impacting balance and well-being.

Motion sickness, often referred to as travel sickness, is a sensation of dizziness that usually occurs when you're traveling by car, boat, plane, or train. Characterized by nausea, dizziness, and vomiting during movement or travel, the condition is often primarily caused by a sensory conflict between what the eyes perceive and what the inner ear's balance signals convey, leading to discomfort and disorientation. While the condition most commonly affects women and children, everyone can get the condition.
Motion sickness can be triggered by various factors that most often include:
The sensory conflict between visual input and the inner ear's balance signals.
Prolonged exposure to motion, such as car rides, boat trips, or air travel.
Reading or focusing on a nearby object while in motion.
Inner ear disorders
Certain medications or medical conditions that affect the inner ear or balance.
While most often temporary, motion sickness symptoms are most often inconvenient and make things far more difficult. Essentially a miscommunication between your sensory organs and your brain, the symptoms will often subside as soon as your body knows what’s going on, but until then will include:
. Dizziness
. Wooziness
. Fatigue
. Nausea
. Vomiting
The main target of motion sickness treatment is to relieve the patient of symptoms at the time they experience motion sickness. More often than not, this may include the practicing of habits during or before travel alongside oral medications. Common steps to manage motion sickness include:
Avoiding activities that trigger symptoms whenever possible.
Reducing the size of meals or avoiding them before traveling.
Practicing relaxation techniques and controlled breathing during motion exposure.
It should be noted that many medical professionals recommend antihistamines for those suffering from motion sickness. However, the antihistamines typically offered will have the side effect of drowsiness. Those taking such medications should avoid operating motor vehicles and machinery.
Nausea and vomiting feel unpleasant, with a persistent urge to expel stomach contents. Symptoms may involve dizziness and salivation. Noticeable distress includes queasiness, stomach discomfort, and retching.

Nausea and vomiting are common gastrointestinal symptoms characterized by a feeling of discomfort in the stomach and the forceful expulsion of stomach contents, respectively. They can be caused by a wide range of factors, including infections, disorders, pregnancy-related conditions, medication side effects, severe headaches or migraines, psychological factors, and more. Especially prominent in pregnant women and those undergoing cancer treatment, nausea and vomiting do not always indicate a greater problem, but can, when paired with other symptoms like pain in the chest or abdomen, a high fever, blurred vision, or blood included in the vomit. In such cases, patients should contact emergency services.
Nausea and vomiting serve as protective mechanisms to rid the body of harmful substances or to respond to various triggers. In some cases, it might be unwarranted, while in others, it may prove life-saving. The most common examples seen in patients can include:
infections (such as viral gastroenteritis or food poisoning),
digestive disorders (like gastritis or irritable bowel syndrome),
motion sickness,
pregnancy-related morning sickness,
medication side effects (such as chemotherapy or opioids),
severe headaches or migraines, and
psychological factors like anxiety or stress.
Nausea and vomiting can appear or feel different depending on whether they are oncoming, in the moment, or ongoing. It's important to note that the severity and duration of these symptoms can vary widely depending on the underlying cause, individual factors, and whether the nausea and vomiting are acute or chronic, with the most common symptoms per each stage including:
Oncoming Nausea:
Nausea often begins with a sense of unease or discomfort in the stomach.
Increased salivation and mouth-watering.
A queasy feeling or a sensation of butterflies in the stomach.
Cold sweats or clammy skin.
Increased heart rate and anxiety.
In the Moment Vomiting:
Persistent and intense nausea.
Salivation and increased swallowing.
Deep breaths and sighs.
Gagging or retching movements.
Forceful expulsion of stomach contents (vomiting).
Relief from nausea immediately after vomiting (for some individuals).
Regular or Chronic Nausea and Vomiting:
Frequent episodes of nausea and vomiting.
Potential weight loss or difficulty maintaining a healthy weight.
Dehydration and electrolyte imbalances.
Fatigue and weakness.
Gastrointestinal discomfort and pain.
Decreased quality of life and impact on daily activities.
Treatment of nausea and vomiting primarily focuses on alleviating symptoms and addressing the underlying cause. Common steps to manage these symptoms include:
Identifying and treating the underlying condition.
Prescribing anti-nausea medications or antiemetics.
Recommending dietary changes and avoiding triggering foods or odors.

A result of injury, natural process, or wear and tear of the body that can range from mild to unbearable. Depending on the severity, accompanying symptoms can include throbbing, reduced mobility, strain, and increased stress overall.

Whether from strain, impact, or another cause, pain relief is one of the most sought-after medical consultations in the United States. With over 20% of Americans suffering from chronic pain alone, it's not unusual for many American men and women to suffer from both temporary and longer-lasting forms of pain. Generally described as uncomfortable sensations in the body that can range from a minor inconvenience to debilitating, pain ranges wildly depending on the cause.
Non-complicated pain, which refers to pain that is not associated with underlying serious medical conditions or complex pathologies, is typically caused by a variety of factors. The most common causes of this condition include:
. Strains
. Sprains
. Overuse
. Arthritis
. Bursitis
. Sciatica
. Neuropathy
. Allergies
. Migraines
. Blunt Force
. Hormones
Call-On-Doc offers treatment for non-complicated conditions specifically characterized by pain. The most common examples of what we offer pain relief treatment include:
Joint Pain: Characterized by discomfort, aching, or soreness in one or more joints, often accompanied by stiffness, swelling, and reduced range of motion.
Arthritis: Marked by chronic joint inflammation leading to symptoms such as joint pain, stiffness, swelling, and decreased range of motion, often worsening over time.
Gout: Manifests as sudden and excruciating joint pain, usually in the big toe, accompanied by redness, swelling, and tenderness, and can be associated with fever and discomfort.
Tooth Ache: Characterized by a sharp or throbbing pain in a tooth, often triggered by hot or cold temperatures, sweet foods, or pressure, and can be accompanied by swelling and discomfort in the affected area.
Back Pain: Presents as discomfort or aching in the lower, middle, or upper back, which can be sharp or dull, and may be associated with muscle stiffness, limited mobility, or radiating pain into the legs or other areas.
Sprains: Typically involve pain, swelling, and bruising around a joint, often resulting from overstretching or tearing of ligaments, and can be associated with reduced range of motion and instability in the affected area.
Headaches: Characterized by pain or discomfort in the head, often with varying intensity, location, and duration, and may be accompanied by sensitivity to light or noise, nausea, and sometimes visual disturbances.
Menstrual Cramps: Involve lower abdominal or pelvic pain that can range from mild to severe, occurring before or during menstruation, and often accompanied by backache, nausea, and discomfort.
In addition to pain relief medication, treatment surrounding non-complicated pain involves reducing the symptoms over time. With acute injuries that include swelling, cold therapy or ice packs are recommended in the first 48 hours or first two days. Always use a barrier between the ice or ice pack, like a towel.
When swelling and inflammation are active symptoms, we recommend against using heat as it can make symptoms worse. However, for sore or tense muscles, stiff joints affected by osteoarthritis, and chronic pain from arthritis or muscle tension, heat therapy can prove effective in reducing the severity of symptoms. Also beneficial when applied to menstrual cramps, heat therapy typically involves using heating pads, warmed towels, a warm compress, and warm baths.

Paxlovid is NOT authorized in the following setting:
NOTE: Paxlovid can only be prescribed if you meet ALL of the following requirements:
Pink eye feels like eye irritation with redness, itching, and discharge, sometimes alongside a sensitivity to light. There may be noticeable discomfort, with discharge and blurred vision being an indication of the condition.

Pink eye, also known as conjunctivitis, is a common eye condition characterized by inflammation and redness of the affected eye’s conjunctiva. Coming in both viral and bacterial forms, children under five years of age make up the majority of cases due to being within close proximity of each other, having still developing immune systems, and still being in the process of learning hygiene. While most cases of pink eye are self-resolving, treatment helps expedite the process and handles cases that require antibiotics.
Pink eye can have various causes, most often being viral, but can also be bacterial and a result of allergens. The most common causes of pink eye include:
Viral Infections: Viruses like adenovirus are a common cause of infectious pink eye.
Bacterial Infections: Bacterial conjunctivitis is often caused by bacteria like Staphylococcus or Streptococcus.
Allergies: Allergic conjunctivitis can result from exposure to allergens like pollen, dust, or pet dander.
Irritants: Exposure to irritants such as smoke, chemicals, or foreign objects can lead to non-infectious pink eye.
Pink eye symptoms are often described as making the eyes puffy, irritated, and crusty on the outside. Discharge from the eyes is possible, with it being a sign of bacterial conjunctivitis. More specifically, symptoms can include:
Redness in one or both eyes.
Itchy or irritated eyes.
Excessive tearing or discharge, which may be clear, white, yellow, or green.
Crusty eyelids, especially upon waking.
Blurred or hazy vision.
Sensitivity to light.
Viral Pink Eye: Viral conjunctivitis is usually self-limiting and does not require antibiotics. Supportive care includes using artificial tears, applying warm compresses to relieve discomfort, and practicing good hygiene to prevent spreading the infection.
Bacterial Pink Eye: Bacterial conjunctivitis is often treated with antibiotic eye drops or ointments prescribed by a healthcare provider. It's essential to complete the full course of antibiotics as directed.
Allergic Pink Eye: Allergic conjunctivitis can be managed by avoiding allergens, using antihistamine eye drops or oral medications, and applying cold compresses to reduce inflammation.
Irritant-Induced Pink Eye: If the cause is irritants, removing the source of irritation, rinsing the eyes with clean water, and using artificial tears can provide relief.

Sinusitis is characterized by the following symptoms: Patients who fail to improve after ≥10 days with home remedies are more likely to have acute bacterial rhinosinusitis.
Strep throat feels intensely painful with fever and difficulty swallowing. Symptoms include redness and white patches on the tonsils. Noticeable discomfort involves severe throat pain, feverish sensations, and potential loss of appetite.
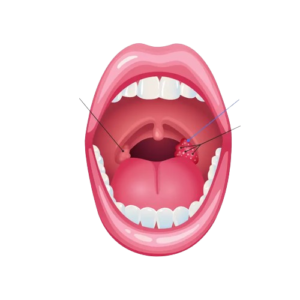
Strep throat (streptococcal pharyngitis) is a bacterial infection that occurs in the back of the throat and the tonsils. The infection often causes inflammation in the throat, which makes it painful to swallow.
People sometimes confuse strep throat with the flu since there can be overlapping symptoms, such as fever, chills, nausea, and vomiting. If your throat feels very painful and swollen or you see red patches or dots in the back of your throat, it’s likely to be strep.
Infection caused by streptococcal bacteria is very contagious. You’re most likely to get strep throat in late winter or early spring. It’s very common in younger children aged 5 to 15, but anyone can get it.
Strep throat is caused by infection with a bacterium known as Streptococcus pyogenes, also called group A Streptococcus.
Factors that increase the risk of getting strep throat include young age (children are more likely to get it) and the season. Most strep infections occur in winter and early spring, in part because people tend to be in close contact during this time of year.
A painful, swollen throat is the most common symptom of strep throat infection.
Other strep throat symptoms include:
Throat pain that develops suddenly
Painful or swollen lymph nodes
Trouble swallowing
Red and swollen tonsils
White patches in the throat
Swelling or redness in the back of the throat
Headache
Nausea/loss of appetite
Stomach pain
Fever or chills
Strep throat is treated with oral antibiotics, such as amoxicillin, Augmentin, or azithromycin. Antibiotics are an effective treatment since strep throat is a bacterial infection. We provide same-day strep throat treatment online. Get antibiotics with no insurance required.
A symptom of the herpes simplex virus, cold sores typically include tingling, pain, and fluid-filled blisters around the mouth or lips. They can be triggered by stress or illness while feeling itchy or painful.

Cold sores, also known as fever blisters, are a common viral infection caused by the herpes simplex virus (HSV). These small, fluid-filled blisters typically appear on or around the lips, but they can also manifest on the nose, chin, or cheeks. Cold sores are highly contagious and can be transmitted through direct contact with the blister or through saliva.
The initial outbreak of cold sores is often preceded by a tingling or burning sensation, which is followed by the formation of small, red bumps. These bumps then evolve into painful blisters filled with fluid. After a few days, the blisters burst, leaving behind open sores that gradually crust over and heal within a week or two.
Although cold sore outbreaks are generally harmless, they can be uncomfortable and unsightly. The primary infection with HSV usually occurs during childhood or adolescence, and the virus remains dormant in the body. Factors such as stress, fatigue, hormonal changes, and a weakened immune system can trigger a cold sore outbreak.
Cold sores, also known as fever blisters or herpes bumps, are primarily caused by the herpes simplex virus type 1 or HSV-1. Upon successful transmission, HSV-1 infects the nerve cells around the mouth and remains in the body in dormant and active states. The disease is most prone to spreading when cold sores or an outbreak is present, but can additionally spread when there are no symptoms in a process known as asymptomatic spreading. The most common mode of HSV-1 transmission is kissing or any oral-to-oral contact.
Symptoms typically begin to appear 2-12 days after exposure. These can include:
Redness and swelling
Small, painful blisters
Pain or discomfort in the affected area
Tingling or itching sensation on spot where cold sores are about to develop
In combination with antivirals like Acyclovir and Valacyclovir, cold sore treatment primarily focuses on managing and reducing the severity and frequency of outbreaks, as well as alleviating symptoms. While there is no herpes cure, the condition can be managed down to a dormant state per each flair-up through treatment and habits that involve lowering stress, reducing spread, keeping the flair-up site clean, etc.
And more...
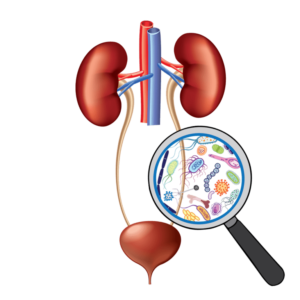
Can UTI be cured?
Does UTI go away on its own?
Do I need UTI testing to get treatment?
Can I treat UTI with over-the-counter medication?
What is the risk for not getting UTI treatment?
Skin infections are a prevalent medical issue that can affect individuals of all ages and backgrounds. They are typically caused by bacteria, viruses, fungi, or parasites infiltrating the skin's protective barrier.
Symptoms of skin infections can vary depending on the type and severity but may include:
The appearance of a skin infection depends on its type, but they can often be mistaken for other skin conditions or allergies.
For example, impetigo may resemble a cold sore, while fungal infections might look like eczema or psoriasis.
Skin infections are caused by microorganisms like bacteria, viruses, fungi, or parasites and can enter through:
Telemedicine has made dermatological diagnosis more accessible. Patients can consult dermatologists remotely using video calls or via photographs. Through telemedicine, patients can share clear photos of skin issues for assessment, and provide detailed information about symptoms, duration, and any relevant medical history. Dermatologists can conduct a visual examination and make a diagnosis.
Includes but not limited to:
Adding {{itemName}} to cart
Added {{itemName}} to cart